What Doctors Don’t Tell You eNews Bulletin- 24/3/2015
93% of men are unable to regain normal erectile function after a radical prostatectomy.
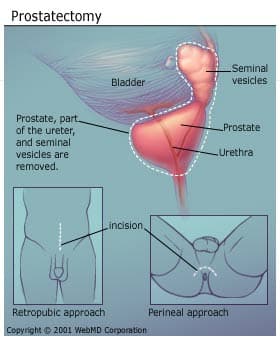
Around 93 per cent of men are unable to have a normal sex life after they have had radical prostatectomy surgery for prostate cancer, a new study has discovered. Regaining normal erectile function after the surgery is “rare”, say researchers from Herlev Hospital in Copenhagen, who surveyed 210 men after they had a radical prostatectomy.
Normal Erection After Prostatectomy Is ‘Rare’
Do Urologists Overestimate Return of Function?
Medscape Medical News
Nick Mulcahy, April 14, 2015
After a radical prostatectomy, it is highly uncommon for a man to have erections like the ones he normally had before surgery, according to a study presented at the European Association of Urology 30th Annual Congress in Madrid.
The researchers reached that conclusion because only 14 patients in the 210-men study (6.7%; 95 %confidence interval [CI], 4.4% – 10.1%) reported that their erections were the same before and after surgery.
“What this work shows is that having an erection as good as before surgery is a rare event,” lead researcher Mikkel Fode, MD, PhD, from the Herlev Hospital in Copenhagen, Denmark, said in a meeting press statement.
There is “controversy” about the incidence of erectile dysfunction after surgery for prostate cancer, the researchers write in their abstract.
The controversy stems, in part, from the fact that the “most commonly used” questionnaire in this setting, the International Index of Erectile Function (IIEF), has not been validated in prostate cancer patients and is vague, the team notes.
To clarify this issue, Dr Fode and colleagues added their own question to the IIEF-5, which is an abbreviated version of the longer questionnaire: “Is your erectile function as good as before the surgery (yes/no).”
They mailed their version of the IIEF-5 to 210 men treated at the Herlev Hospital who completed the questionnaire an average of about 23 months after surgery.
Even without the extra question, IIEF-5 scores indicated that the men (mean age, 65 years) were struggling.
Having an erection as good as before surgery is a rare event.
For men who completed the IIEF-5 questionnaire before surgery, the mean score was 21.7 (95% CI, 20.6 – 22.9). After treatment, the mean score dropped to 9.9, with a lower score indicating more dysfunction (95% CI, 8.6 – 11.3).
The researchers also collected information on the use of erectile aids.
Of the 189 men who did not use aids before radical prostatectomy, 83 started to do so after surgery. Specifically, 58 patients began using phosphodiesterase type 5 inhibitors, 17 began using injection therapy, five began using urethral suppository alprostadil (MUSE), one began using a vacuum erection device, and two received a penile implant.
Notably, the 49 patients (23.3%; 95% CI 18.9% – 28.5%) who did not use erectile aids showed no decline in IIEF-5 score.
ED Induced by Prostate Biopsy Likely ‘Underestimated’
Nick Mulcahy, October 01, 2015
The various degrees of erectile dysfunction (ED) that occur after prostate biopsy with a needle through the rectum wall have “probably been underestimated,” according to new research.
A new study showed a “significant decrease” in the erectile function score of most men after biopsy, and the drop was independent of age, cancer diagnosis, and previous biopsy status, report the study authors, led by Katie Murray, MD, from the University of Kansas Medical Center in Kansas City.
Although ED was recognized as a complication of prostate biopsy as early as 2001, it has not been well-established by data, unlike potential adverse events such as hematuria, pain, voiding dysfunction, and infection.
In their prospective study, Dr Murray and her team used a standard test — the International Index of Erectile Function (IIEF-5) — to evaluate 220 men with elevated levels of prostate-specific antigen (PSA) who underwent a transrectal-ultrasonography-guided prostate biopsy.
In the study cohort, median IIEF-5 score was significantly lower 1 week after biopsy than at baseline (15.5 vs 18.2; P < .001). And the score remained significantly lower at 4 weeks (17.3 vs 18.4; P = .008) and 12 weeks (16.9 vs 18.4; P = .004).
The team does not, however, say that the needle caused physical damage in this nerve-intensive area that led to ED. “The exact cause of this effect is yet to be determined,” they write.
The study was published in the August issue of BJU International.
“Psychological stress” likely contributes to the ED, writes Brian Helfand, MD, from the University of Chicago, in an accompanying editorial. The men in this study who had a benign biopsy had a fairly quick return to baseline in terms of their erectile function (after 1 week, as a group), even though some men reported lower scores for up to 3 weeks.
Dr Helfand points out that a study he was involved in showed that a diagnosis of prostate cancer “can influence a man’s erectile function after prostate biopsy” (BJU Int. 2013;111:38-43).
The literature on this subject is mixed, with some studies finding and some not finding that biopsy induces ED, he adds. Nevertheless, Dr Helfand suggests that “patients should be counseled on the possibility of relatively short-term (‘acute’) changes in erectile function.” Dr Murray and her team say the same thing.
This single-group study could have been stronger in terms of its evidence, said Clint Bahler, MD, from Indiana University in Indianapolis, who was not involved in the study but was asked to comment on the findings.
“They should have followed another group of [healthy] men with elevated PSA who did not get biopsy to compare, for instance,” he told Medscape Medical News.
Like Dr Helfand, Dr Bahler pointed out that men who had a benign biopsy (67% of the group) had relatively transient ED, compared with those who had cancer detected.
For the patients who did not get a diagnosis of prostate cancer, median IIEF-5 score was lower only at the 1-week follow-up (P < .001). But for those with prostate cancer detected, the median score was lower at 1 week (P < .001) and at 12 weeks (P = .001) after biopsy.
Notably, there is no detailed breakout of scores for the benign group. “They should give us the scores for the benign group, but these are censored, which is suspicious,” said Dr Bahler.
Dr Helfand, Dr Bahler, and the investigators all suspect that longer-term ED might be related to a host of factors, including stress, a diagnosis of cancer, and age.
As Dr Murray’s team puts it, “the exact mechanism of this decline in IIEF-5 score for these patients is most likely multifactorial in nature and many factors — including psychogenic causes, fear of results, anxiety related to biopsy, and even anatomical considerations including nerve damage and hematoma — have potential in being related.”
At baseline, the average age was 64 years, and ED status was reported as nonexistent by 39% of the men, as mild by 22%, as mild to moderate by 15%, as moderate by 10%, and as severe by 14%.
Age appears to play a role in how men do in terms of their erections after undergoing prostate biopsy, the investigators report.
For men younger than 60 years, median IIEF-5 score was lower only at the 1-week follow-up (P = .015). But for men 60 years and older, scores were lower at 1 week (P < .001), 4 weeks (P = .024), and 12 weeks (P = .005).
The investigators also used the International Prostate Symptom Score (IPSS) questionnaire to evaluate the men. They focused on data related to lower urinary tract symptoms, and found that there was a significant change at weeks 1 and 4, but not at week 12. In other words, in this cohort of men, symptoms, on average, improved by week 12.
The study authors, Dr Helfand, and Dr Bahler have disclosed no relevant financial relationships.
BJU Int. 2015;116:164, 190-195. Editorial, Abstract
Nervous wait to get back in the saddle
PUBLISHED: 24 Jul 2013, Australian Financial Review
A leading urologist describes erectile nerves as a diffuse network, almost like this spider webbing.
Financial Review health editor Jill Margo recently returned from a Churchill Fellowship abroad where she researched sexual rehabilitation following surgery for prostate cancer. In the first of a three-part series, she lifts the lid on nerve-sparing surgery. When it comes to surgery for prostate cancer, men want to achieve the trifecta. They want to emerge cancer-free, continent and potent. In most cases, if their cancer is operable, they achieve the first two. The third, however, often remains elusive. There are complex reasons for this – but the most important one relates to their erectile nerves. If these nerves are removed during surgery, they have no chance of regaining natural potency. But if these nerves are spared, theoretically there is a good chance. The reality, however, is that most men who have nerve-sparing surgery don’t regain what they had and some are left with nothing. This is confusing and can be devastating.
Although the nerves are described as occurring in bundles, they are not like thick wires hanging between telegraph poles. Rather, they form a network in a veil that is so fine it is hard to see with the naked eye. In the past, there was no thought of sparing nerves. Men were grateful just to have their cancerous prostate removed. That was the only focus of the surgery and there was so much blood in the operating field that 25 per cent of them emerged incontinent. All emerged impotent.
When ways were found to control the bleeding, continence rates improved dramatically, but impotence remained the same.
Medical text books taught that the erectile nerves ran through the prostate, so when the prostate was removed it was understood that the nerves went with it, and that was the end of natural potency. An unexpected reprieve No one questioned this until 1977, when a urologist at Johns Hopkins Hospital in Baltimore encountered the unexpected. Three months after a radical prostatectomy, a patient reported he was potent. This obviously meant his nerves had not been removed with his prostate. So where were they? About four years later they were located outside the prostate, together with tiny blood vessels in the so-called veil. This was a cause of great interest and it was thought that if these nerves could be preserved during surgery without compromising the curative intent of the operation, then surely the man could be potent. And if they could be partially preserved, perhaps he could still be potent.
In 1982, the first deliberate nerve-sparing procedure was performed and, since then, the method has been revised and improved several times.
Nerve-sparing was a major development in prostate surgery and brought high expectations. It is now widely available and, every day, men around the world receive the good news that their operation went well and all their nerves were spared.
But despite this, only a few naturally regain potency and it is rare for them to regain the same level of function they enjoyed before the operation.
No one is certain of the reasons but there are several possible explanations.
The first is that all the nerve fibres may not have been spared in the way the man and his surgeon believed they were. The visibility problem for the surgeon means it can be difficult to assess just how much was saved.
Celebrated urologist Peter Scardino of Memorial Sloan-Kettering Cancer Center in New York has described the process of sparing the erectile nerves as the equivalent of “neurosurgery” and says 90 minutes in the operating theatre is not enough to protect these nerves.
When completely spared, they should have the capacity to repair themselves. But Yoram Vardi, a leading neurourologist and professor at Rambam Health Care Campus, Haifa, Israel, says somehow 40 per cent of men who have full nerve-sparing, have no erection.
There is always a subjective element to nerve-sparing. To all present, the surgeon might perform a magnificent operation but there is little objective data to confirm what has been preserved. Vardi says the problem is visibility. “You don’t see the nerve but, because you are close to the prostate, you know it should be there. You see “a bundle”, it is very diverse in different patients and is not a defined anatomical structure that you can be sure about.
“With complete nerve-sparing, men should be potent a month later, but we know 90 per cent are not even able to have an erection after surgery.”
He suggests that something may be wrong with the definition of total nerve-sparing and that, in many cases, it may be partial. The second possible explanation is that the nerves were spared but were injured during surgery.
Some explain the injury by describing the prostate as a hard-boiled egg and the veil as the membrane covering the egg. In this case, it only covers part of the egg.
This membrane must be kept perfectly intact while it is peeled back so the prostate can be removed. The nerves within it are exquisitely sensitive and can be damaged even in the most skilled hands with the most delicate peeling. There is traction, they sustain percussion injuries and can be badly affected by energy used in the operating field, such as heat from cautery.
One leading urologist explained the nerves as a diffuse network of very fine fibrous webbing, almost like spider webbing, encased in a fascia and mixed with blood vessels. Preserving them without damage is extremely challenging. Another preferred the analogy of a two-layered tent with the nerves lying between the layers. As long as both layers are preserved during surgery, the nerves are probably preserved too.
But not even pathologists, who have time to examine the prostate in detail on the laboratory bench, can be certain about the effectiveness of a nerve-sparing procedure.
Ronnie Cohen, professor at the University of Western Australia and a foremost prostate pathologist, says nervesparing doesn’t always correlate with potency.
“It might look like a very good nerve-sparing procedure but we don’t know how the tissue was handled. Sometimes we receive a prostate with a lot of nerve tissue and we think, ‘oh no, this is a disaster for potency’, but the patient inexplicably regains his potency. There are many variables.” Nerve-sparing is always done with the proviso that cancer cure comes first. If the tumour has reached the nerves, they have to be excised, at least on that side of the prostate.
Over the years, there have been attempts from many angles to try to improve the outcome for erectile nerves. Could they be bolstered before surgery, could they be stained for visibility, could they be stimulated and mapped, could they be protected during surgery and could their recovery afterwards be accelerated?
So far researchers have produced nothing definitive but work is continuing.
Once they are damaged, erectile nerves can take two years to recover. Recovery has been reported beyond this but some experts attribute this to the man’s increase in confidence. The third explanation is that while the nerves slowly repair themselves, the erectile machinery falls into disuse. The tissues gradually undergo change, they become fibrotic and scarred, and this damage cannot be reversed. When the nerves are ready to fire again, the machinery can no longer respond. The highest aim of penile rehabilitation following prostate surgery is to keep the machinery running until the nerves recover so that it can run on its own, or with just a little assistance.
Doctor, I need those nerves:
John Mulhall, an acknowledged leader in rehabilitation after prostate cancer, advises men to begin their surgical journey with their eyes wide open.
As professor and director of the male sexual medicine program at Memorial Sloan Kettering Cancer Center, New York, he says it is vital they communicate the importance of their potency to their surgeon. “Emphasise the need for the surgeon to do the best job possible. At MSKCC, which is a paragon of good prostate surgery, if you have baseline erectile dysfunction, you are five times less likely to get a nerve-sparing procedure.” “The surgeon thinks, ‘oh well, he’s got erectile dysfunction anyway so he doesn’t need those nerves. Why take the time and effort?’
“That’s human nature. But I say, of course you need those nerves.
“The other problem is that, after his diagnosis, a man asks around and goes to see a big-name surgeon. Two weeks prior to surgery his erectile function is not as good as it was six months before because he is stressed and anxious. The surgeon says ‘ah, his erections are not good’. Then the man doesn’t get nerve-sparing although, in fact, his machinery was perfect.”
World authority on erectile dysfunction, Arthur L. Burnett, professor and neuro–urologist at Johns Hopkins School of Medicine in Baltimore, holds a similar view.
He says some surgeons today are too ready to dismiss a man who is somewhat dysfunctional and do not do their best to preserve the modest level of function that he may have.
“I believe we need to preserve nerve function under all circumstances – as long as it does not compromise disease control. Irrespective of his initial presentation, the man’s potential quality of life should be maximised.” He says some patients don’t want to do anything at the time of the operation but come back six months later when their continence is good and their health is back and ask “where are my erections, doctor?”
The Australian Financial Review
One-Day Couple Group Intervention to Enhance Sexual Recovery for Surgically Treated Men With Prostate Cancer and Their Partners
A Pilot Study
Researchers evaluated the acceptance and effectiveness of a group intervention that provided education about post-prostatectomy sexual recovery and peer support for couples. Couples valued the intervention and retained the information. Partners became accepting of erectile dysfunction and communicated more openly about upsetting topics.
Introduction
Prostate cancer affects one in six men in the United States (U.S.) and represents 40% of all male cancers (Hewitt & Stovall, 2006; Jemal, Siegel, Xu, & Ward, 2010). Between 35% and 64% of men diagnosed with moderately differentiated prostate cancer (Gleason sum 5–7) who are 55 to 69 years of age undergo prostatectomy as their initial definitive treatment (Miller, Gruber, Hollenbeck, Montie, & Wei, 2006). Sexual problems tend to ensue and reduce the quality of men’s lives (Benson, Serefoglu, & Hellstrom, 2012). Several years after treatment, as many as 50% of survivors consider sexual problems to be bothersome (Sanda et al., 2008). Sexual dysfunction not only affects the man with cancer but also his sexual partner (Bruun, Pedersen, Osther, & Wagner, 2011; Tanner, Galbraith, & Hays, 2011). It has been documented that as many as 44% of prostate cancer survivors’ partners have sexual problems (Sanda et al., 2008), but the inclusion of partners in studies is only recent.
Most of the research on providing help in sexual recovery to prostate cancer survivors has focused on medical interventions (Incrocci, Slob, & Hop, 2007; Mazzola & Mulhall, 2011; Montorsi et al., 2010). Psycho social approaches are only emerging. Psycho-educational and supportive interventions have been especially helpful to partners in improving their appraisal of the illness and enhancing their sense of coping (Manne et al., 2004; Northouse et al., 2007). Interventions that have included partners and focused more specifically on erectile recovery have had positive but short-term results (Canada, Neese, Sui, & Schover, 2005; Davison, Elliott, Ekland, Griffin, & Wiens, 2005). Interventions addressed to men alone have also shown promise: group treatment (for men only) aimed at reducing distress for men after prostate cancer treatment resulted in improved sexual function in men who were coping less well initially (Molton et al., 2008), and the inclusion of counseling with medical treatment improved men’s adherence to penile injection therapy (Titta, Tavolini, Moro, Cisternino, & Bassi, 2006).
A randomized trial that examined the effectiveness of in-person versus Internet-based counseling for sexual recovery after prostate cancer revealed comparable effects of both interventions (Schover et al., 2012). Both male and female sexual function was affected by baseline female sexual function. Women whose sexual function was low at baseline improved. Male sexual function improved more if their partners’ sexual function was higher. Men who completed the intervention improved more than those who did not. An intimacy enhancing intervention was particularly effective with couples who had fewer psychological resources (Manne et al., 2011).
Latini, Hart, Coon, and Knight (2009) carried out a review of interventions and found that most psycho-social interventions focus primarily on psychological adjustment rather than on sexual recovery. They also suggest that studies should include more diverse samples, particularly in regard to sexual minorities. A more recent review of interventions specifically aimed at evaluating interventions designed to improve men’s sexual function and couples’ sexual relationships found that interventions tended to help men’s sexual function, but did not improve partners’ sexual function or couples’ sexual relationships (Chisholm, McCabe, Wootten, & Abbott, 2012).
Sex and secret men’s business

When Brisbane woman Jill Costello received treatment for breast cancer seven years ago, she found herself surrounded by expert care and support. Her ”fairy godmother”, a breast-care nurse, just made things happen. Her questions were fully answered, her doctors went out of their way to make sure she had proper advice and every possible aid to her recovery.
Four years later, when her husband, Brian, had surgery for prostate cancer, the couple discovered they were on their own. Questions about lasting side effects from the surgery were fobbed off and Jill found herself Googling late into the night, reading up on risks of incontinence and erection problems resulting from damage to the penile nerves.
”Even when I made an appointment to see the urologist myself, he simply warned there could be difficulties but gave no advice on what to do or where to go,” she says.

The couple muddled through themselves, asking around until they found one of the few local doctors offering specialist help with the erection recovery process and a physiotherapist for the incontinence.
With her daughter Leah, Jill now runs the organisation ManUp!, which raises money to train more prostate cancer nurses. There are only 12 specialist prostate cancer nurses in Australia (with new federal funding for an additional 13 next year) compared to 85 for breast cancer. Yet, more men are diagnosed each year with prostate cancer than women with breast cancer (18,560 compared with 14,560 in 2012, according to the Australian Institute of Health and Welfare).
ManUp! hears regularly from men whose urologists have shown no interest in what happens to their patients after prostate cancer treatment. One man left impotent and incontinent after his robotic surgery was told the doctor’s job was simply to deal with the cancer.

”That’s crazy. It’s like a knee surgeon not caring whether the man can walk again. It’s appalling how few urologists are making sure men have the help they need to regain erections and continence, yet the impact of these problems can be just as devastating to a man as a mastectomy can be to a woman,” Jill says.
This week a world congress on prostate cancer is being held in Melbourne, with up to 300 urologists among 1000 delegates attending from Australia and overseas. Although there are sessions on sexual functioning and continence, many urologists choose instead to attend talks on the latest cutting-edge treatments or diagnostic techniques.
”We have got better with the technical aspects of the surgery to remove the prostate and preserve function, but I think we have a long way to go with all aspects of rehabilitation, including the psychology of facing a serious illness, urinary incontinence and erectile failure,” says Prem Rashid, a urologist and associate professor at the University of NSW, who has spent more than 15 years involved with urology training.
Rashid points out that it’s hard for busy practitioners to keep up to date with the recently developed erection treatments. ”It’s also a two-way street, with some men finding it difficult to talk about these issues,” he says.
”We really need to be proactive in helping our patients,” says Dr Darren Katz, a urology fellow at Fremantle Hospital and a speaker at the conference. Katz is just back from working with world experts in erectile dysfunction and incontinence at New York’s Memorial Sloan-Kettering Cancer Centre.
Next year he will open a specialist men’s health clinic in Melbourne working with Dr Christopher Love, one of Australia’s most experienced penile implant surgeons and experts in the erection recovery process.
As he’ll explain at the conference, there’s a growing international consensus that men should be treated with pro-erection medications rather than just hoping erections will return years after prostate cancer surgery. Ideally, men should start treatment as soon as possible to maximise their chances of regaining natural erections.
”Regular erections supply oxygen to the penis through increased blood flow. This helps to prevent scarring and keeps erectile tissues healthy until the erection nerves have a chance to recover,” he says, explaining this is necessary even if surgery has spared these nerves. Treatments such as radiation can cause similar damage.
Lost erections aren’t the only problem. ”Some men leak urine when they orgasm and up to 70 per cent report some shortening of the penis after prostate surgery, a major concern for many men,” says Katz, explaining this shrinkage can be due to scarring of erectile tissue and the casing of the erection chambers, which can also cause abnormal bending of the penis.
Katz will speak at the conference about ”penile rehabilitation” aimed at preventing this shrinkage and helping restore erections. ”This usually involves a combination of regular doses of one of the erection pills like Viagra, Cialis or Levitra and, if needed, injection therapy a few times a week and possible use of a vacuum erection device.”
Ideally the man’s erectile functioning is assessed before and after prostate cancer treatment, leading to an individually tailored treatment plan.
”Many men are really nervous about the idea of injecting the penis, but if they are carefully taught how to use the injection medication that’s right for them they discover these treatments are really effective and quite painless,” Katz says.
But that’s just the problem. Most men receiving treatment for prostate cancer receive little help for their erection problems, let alone careful assessment to determine the exact prescription they need.
Most experts in the field find many men respond better to injection therapy involving a combination of drugs that are available only from compounding chemists. There are pre-mixed injections available, but for many men premixed drugs are less effective and more likely to cause pain.
With only about 15 compounding pharmacies in Australia with the sterile rooms required to produce these drugs, many of these pharmacists report these drugs are being prescribed by only a handful or so of urologists in each capital. That shows how few of our country’s 400 urologists are offering comprehensive treatments for sexual rehabilitation.
Some urologists do refer patients on to ED specialists, like Love, or Sydney sexual health physician Michael Lowy but experts in this area all acknowledge most of their referrals are coming from a small group of doctors.
”Most patients who find their way to me have searched for proper help themselves after prostate cancer treatment,” Lowy says. ”Men often tell me their urologist gave them little or no advice whatsoever about what to do about their loss of erections.”
Professor Mark Frydenberg, vice-president of the Urological Society of Australia and New Zealand, says that while isolated anecdotal cases of dissatisfaction with urologist management may occur, ”in the majority of cases men receive appropriate and empathic care to recover their sexual functioning following prostate cancer treatments and there is no hard evidence to the contrary”.
He does suggest that if a patient is not getting the help they need, they should seek another opinion. ”Issues surrounding erectile dysfunction following prostate cancer treatments are complex and multi-factorial and often require the help of a multidisciplinary team including urology nurses and psychologists with special expertise in both cancer and sexual health.”
Many of these men end up in the hands of shonky organisations that charge thousands of dollars for often ineffective treatments, such as that provided by Jack Vaisman’s Advanced Medical Institute, which makes more than $70 million a year ”treating” Australian men. Vaisman is facing a ban from corporate life for ”unconscionable conduct” after an action by the Australian Competition and Consumer Commission.
There have been many reports about this company’s practices: lies about the effectiveness of its treatments; salespeople illegally withdrawing money from a patient’s credit cards; dubious tactics to avoid money-back guarantees; failure to properly check medical histories or warn of dangerous side effects. The clinics offer compound injection treatments but charge up to 10 times the cost of legitimate compounding pharmacies with no proper medical examinations or education.
”Vulnerable men end up paying big money for ineffective treatments because they aren’t getting the help they need from their own doctors,” says David Sandoe, national chairman of the Prostate Cancer Foundation of Australia. His organisation is planning national education campaigns aimed at giving men the information they need and encouraging them to choose doctors who care about their sex lives.
It’s an issue close to Sandoe’s heart. With his wife Pam, he’s spent years talking publicly about his own experiences with various erection treatments after his prostate cancer surgery. This remarkable couple regularly entertains conference rooms full of doctors and consumers with stories of the first time they used the injection therapy. David rushed home from the doctor’s surgery with a full erection only to discover their house was full of painters – they were in the middle of a renovation. That didn’t stop them. ”With a couple of lame excuses we made it to the bedroom and put ‘it’ to good use,” Pam says.
The couple are regular travellers and found the vacuum pump led to funny moments at airports as they explained to embarrassed customs officers exactly what it was. David is now the proud owner of an inflatable penile prosthesis, which works exceptionally well, even though the noise of the pump as it pushes liquid into the penis still gives Pam the giggles.
The Sandoes were lucky in their choice of urologist, as Sydney-based Phillip Katelaris provides a comprehensive service that includes a psychologist and nurse educator to explain erection treatments and teach pelvic floor exercises essential for incontinence.
Many men are forced to suffer the humiliation of spending years wearing nappies or pads due to incontinence after prostate cancer treatments. Research from the Cancer Council NSW found five years after a radical prostatectomy, three-quarters of the men have erectile dysfunction and 12 per cent are still incontinent.
Associate professor David Smith, one of the authors of the study, suggests the erectile dysfunction numbers are twice what you’d expect through the ageing process and the incontinence figures are also too high.
Shan Morrison, director of Women’s and Men’s Health Physiotherapy in Malvern says: ”Most men aren’t aware that they needn’t live with long-lasting embarrassing continence problems. A physiotherapy pelvic floor rehabilitation program usually results in continence within six-to-12 weeks of prostate cancer surgery.”
Sydney psychologist Patrick Lumbroso, who is undertaking doctoral research into erection problems after prostate cancer surgery, is frustrated at how poorly these issues are handled: ”Problems such as incontinence and erectile dysfunction can have a devastating impact on a man’s confidence and masculine self-image, leading to depression, relationship problems and sexual difficulties for the partner.”
His research reveals why so many men in this circumstance fail to receive proper advice on erection treatments, finding most men are given little or no information by their urologists, and if they are given advice it is often inaccurate and poorly handled.
”One doctor asked his patient, ‘Have you ever considered jabbing a needle into your penis to get an erection?’ That was hardly a sensitive approach given the squeamishness of most men to using injections,” Lumbroso says.
Lumbroso also provides counselling to couples, helping them adjust to the impact of prostate cancer treatments on their sex lives. Like most experts in the field, he would like to see much more being done to reach people in this situation. ”It’s tragic how many couples are left floundering on their own when so much could be done to help them resume sexual intimacy.”
Bettina Arndt is a former sex therapist and social commentator.